Focusing on Healthcare Instead of "Sick Care"
“The doctor of the future will give no medicine but will instruct his patient in the care of the human frame, in diet and in the cause and prevention of disease.” - Thomas Edison, 1902
What Should Healthcare Be?
This prescient quote is the genesis behind the idea of Healthcare, which proactively creates optimal health by preventing chronic and acute conditions from occurring in the first place. Opposed to the status quo "sick care" model, which reactively treats emergencies or illnesses.
Problems with “Sick Care”
Ultimately, the current U.S. “sick care” system is damage mitigation and ranges from treating chronic conditions such as cancer, heart disease, and diabetes to the repair of acute or life-threatening situations. The goal should be to find conditions or diseases when they are asymptomatic. We need to catch a disease early, in its infancy, before more invasive options that require hospitalization or surgery become the only option.
The Healthcare mission has to be in the form of truly “preventative care” and not “sick care”. The ‘you break, I fix’ reactive care model is an outdated paradigm and, again, our aim needs to be centered around prevention. Stopping or improving a current illness is imperative and achieved through closing Care Gaps. Furthermore, “preventative care” necessitates early identification of conditions before they become a health complication or life-threatening. With the proper Care Gap reminders and help with social determinants of health measures, an individual’s health overall can be managed, stabilized, and at times, adverse events can be avoided.
Today, older adult care is not aligned with a true member-centered medical home model where the care is comprehensive, coordinated, and preventative. Improving access to care and accountability would strengthen the physician/plan-member relationship and lead to better health outcomes for these individuals.
Move Towards Preventative Care for Medicare Advantage Members
For people covered by Medicare plans, the Annual Wellness Visit (AWV) is a form of preventative care that can drastically increase overall health. Annual Wellness Visits are yearly appointments with a primary care physician to create or adjust preventative plans for members. Annual health care costs for members who go to an AWV are, on average, lower than those who do not. In a recent study, it was found that patients who received an AWV experienced a 5.7% reduction in adjusted total health care costs.
While Medicare Advantage enrollees are taking advantage of AWVs at a growing rate only a quarter of enrollees complete an AWV. Beyond this visit, there are still vital Care Gaps that need to be identified, addressed, and closed. Annual Wellness Visits can only give a physician a partial glance of the preventative care that their patient needs. Having information on a patient’s environmental and social factors can help build a more holistic care plan than the information gathered through a doctor’s office.
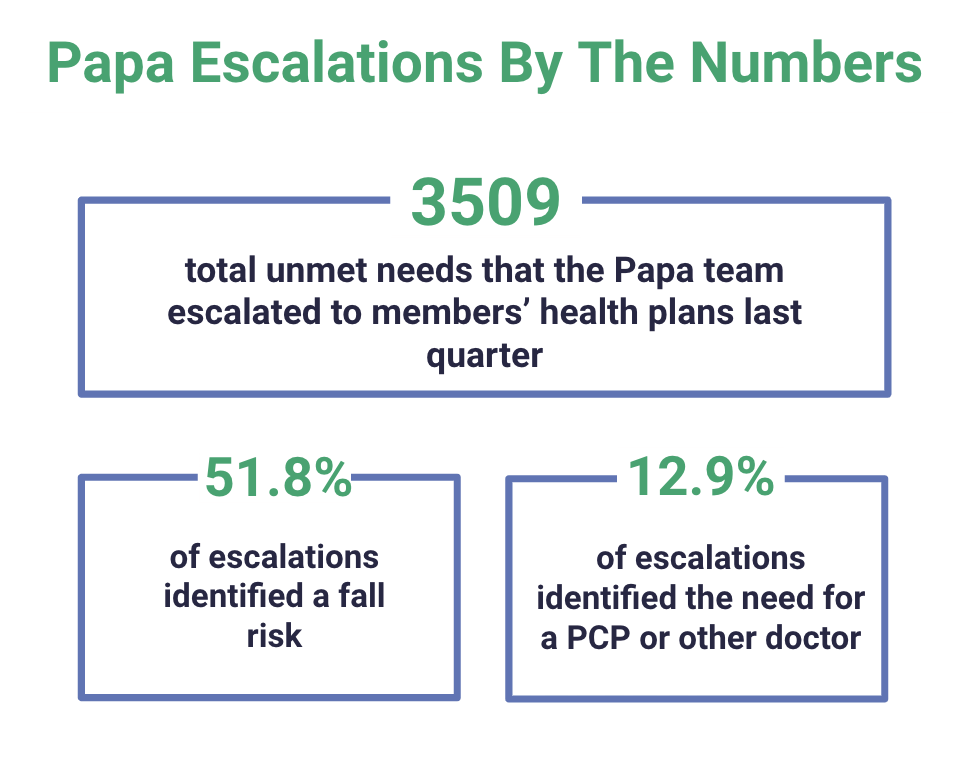
Papa pairs older adults and families with “Pals” who offer companionship, transportation services, household help, and more. These Pals are also trained to identify and escalate unmet needs to help resolve health risks for older adults. In quarter 3 of 2021 alone, Papa has identified and notified the members' health plans of over 3000 care gaps. Of these escalations, 51.8% were for fall risks. Other examples of gaps identified were members needing a PCP, unsafe environments, financial concerns, barriers to medication adherence, and behavioral health challenges. Papa works with health plans to not only identify these health risks, but has recently introduced a new service, Care Concierge, that helps to mitigate and resolve the Care Gaps.
At Papa, we believe the best treatment plan is lifestyle modification. This means we need to discover the health risks early enough so they can still be influenced positively with straightforward actions. Examples of this are improving diet, implementing exercise, and maintaining a sleep schedule; or measures such as eliminating smoke, drinking in moderation, and reducing stress. Our Pals work with members to build trust and relationships and then help them make changes that will impact their health vastly.
Over the years, we have noticed that members who spend more time with Pals are living happier, less lonely lives. We are helping members get to their Primary Care Physician, enabling them to identify chronic diseases before they lead to a catastrophic event. These patients are having a lower incidence of chronic conditions and are also showing an improvement in their UCLA loneliness score. Older adults deserve more and at Papa, we treat every person like they are someone’s loved one, someone’s mom, dad, or grandparent. We are their family on-demand.
About the Author
 Dr. Rajiv Patel, MD
Dr. Rajiv Patel, MD
VP of Clinical Operations at Papa
Dr. Rajiv Patel leads the clinical efforts at Papa to help facilitate patients receiving medically appropriate care. Dr. Patel leads the Care Concierge team at Papa in which he focuses on prevention of disease along with social determinants of health. His team evaluates members for social determinants of health through a proprietary data driven model developed by Papa based on years of experience leveraging clinical and non-clinical data.
Combating Loneliness and Social Isolation Among Older Adults
For America’s older adults, loneliness is all too common and this lack of connection can have life threatening consequences. Find out how Papa can decrease loneliness and improve the health of older adults by downloading our free white paper today.